Autoantibodies: new treatment options and challenges in neurology
3rd Congress of the European Academy of Neurology in Amsterdam
Amsterdam (ptp002/25.06.2017/08:00) Memory loss, epilepsy, psychiatric disorders and movement disorders are some of the complaints and conditions that we now know can be triggered by autoantibodies and which respond clinically to immunotherapies. Antibodies usually protect organisms against infections or foreign bodies, but autoantibodies are those that attack the body's own tissue. The brain was not previously thought to be susceptible to autoantibodies because it is protected by a blood-brain barrier, but now the role of autoantibodies targeting certain brain proteins is well recognised. "These diseases are not common, but they can lead to serious conditions developing over a matter of days or weeks," said Prof Angela Vincent of the University of Oxford at the 3rd Congress of the European Academy of Neurology (EAN) in Amsterdam.
Research pinpoints targets
The advances depend on identification of the autoantibodies that can cause brain disease: these antibodies attack different receptors and channels that are membrane proteins of neuronal cells in the central nervous system. These targets include NMDA and other glutamate receptors, inhibitory receptors such as GABA and glycine receptors, and LGI1 and CASPR2, two proteins that help control neuronal excitability. Other antibody targets are found on the glial cells and found in patients with demyelinating disorders. The new knowledge plays a significant part in early recognition and diagnosis. "In many cases of acute or subacute neurological disorders, the possibility of one of these specific antibodies needs to be considered, and if identified, immunotherapy is likely to be effective," Prof Vincent stated.
Immunotherapy as a new treatment option in rare forms of epilepsy
The identification of these antibodies helped to draw attention to a new form of seizure: the patients are affected by frequent, brief dystonic movements of the arms and face. These "faciobrachial dystonic seizures" are thought to be caused by autoantibodies against the LGI1 protein. Dr Sarosh Irani in Oxford, who led this study, has found that the patients respond well to immunotherapy, with the seizures often disappearing within weeks. Previously these patients would have developed a limbic encephalitis with profound amnesia, but prompt immunotherapy may protect the patient from developing this more severe condition.
Although the link between LGI1, and other antibodies, and limbic encephalitis is clear, the diagnosis of the condition does not have to be dependent on a positive antibody test. "There are now published guidelines for diagnosing patients with autoimmune forms of encephalitis - by means of careful assessment of the syndrome, and with MRI and CSF tests that are available in most institutions."
Could immunotherapy be effective in treating some of the typical epilepsy sufferers who do not respond to conventional medication? "We and others are studying this question; autoantibodies could be the cause of a small per cent of typical epilepsy cases, but research is needed to see whether the patients respond to immunotherapies," Prof Vincent said.
Autoantibody screening
Antibody screening has become widespread with commercial tests available, but it is not always easy to determine for which patients screening is required. More new antibodies are being discovered in blood serum and spinal fluid. Some are relatively common, while others are very rare. Although the link between specific autoantibodies and the neurological features is usually well established in the first description, these features, such as seizures or amnesia, are common to many other more common conditions. This is leading to a large rise in the number of antibody tests requested and inevitably there will be some results that are not helpful. "The clinicians need to decide which antibodies to test for, whether positive results are clinically relevant and, if so, how aggressively the patients should be treated. This can be difficult," Prof Vincent explained.
One example is antibodies against the N-methyl-D aspartate receptor (NMDAR), which can cause a very well described clinical syndrome with movement disorder, but often begins with psychotic behaviour. The condition, identified by Prof Josep Dalmau in the University of Pennsylvania, usually goes into remission if treated using immunotherapy, although often only after weeks to months. The difficulty lies in the fact that the presenting clinical characteristics of the psychosis are not obviously different from those of patients with typical psychosis without the NMDAR antibody. Should all patients presenting with a first episode of psychotic illness have the antibody test? "Results of studies so far have been variable and opinions on the potential value of such testing range from scepticism to enthusiasm," Prof Vincent commented. In her view, it is still too early to judge whether using comprehensive "autoantibody screening" in patients with isolated seizures, psychosis or cognitive dysfunction would make sense in the future.
Sources: Josep Dalmau, Angela Vincent. Do we need to measure specific antibodies in patients with limbic encephalitis? Published online before print January 6, 2017; Lennox et al. Prevalence and clinical characteristics of serum neuronal cell surface antibodies in first-episode psychosis: a case-control study. The Lancet Psychiatry, Vol. 4, No. 1, 01.01.2017; James Varley, Angela Vincent, Sarosh Irani. The role of adaptive immunity in Parkinsonian syndromes. ABN Abstracts 167, 2016 ABN Annual Meeting; Oxford Epilepsy Research Group: Autoantibodies In Epilepsy: Research Improving Patient Care; Dawes, John M.; Vincent, Angela. Autoantibodies and pain. Current Opinion in Supportive & Palliative Care: June 2016 - Volume 10 - Issue 2; Angela Vincent. Developments in autoimmune channelopathies. Autoimmunity Reviews 12 (2013) 678-681
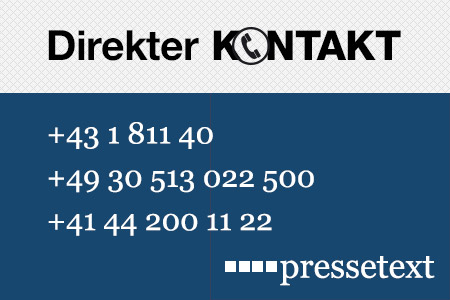
(end)| Aussender: | Bettschart & Kofler Kommunikationsberatung GmbH |
| Ansprechpartner: | Dr. Birgit Kofler |
| Tel.: | +43 676 63 68 930 |
| E-Mail: | kofler@bkkommunikation.com |
| Website: | www.bkkommunikation.com |